It’s 2 a.m. The house is quiet, except for the sound of a small, persistent cough coming from your child’s room. You place a hand on their forehead and feel the unmistakable heat of a fever. Your heart sinks a little. A quick trip to the 24-hour pharmacy follows, where you find yourself standing under fluorescent lights, staring at a wall of brightly colored boxes. “Multi-Symptom Cold & Flu,” “Nighttime Cough,” “Fever & Pain.” The choices are overwhelming, and the weight of making the right one for your sick child feels immense.
If this scene feels familiar, you are not alone. Every parent has faced this moment of uncertainty. This guide is designed to be your calm, clear, and comprehensive partner in navigating the world of pediatric over-the-counter (OTC) medicines. We will walk you through it step-by-step, transforming that middle-of-the-night worry into well-prepared confidence. Because here’s the secret: the most powerful tool for keeping your child safe isn’t in the medicine bottle itself; it’s the knowledge you arm yourself with
before you even twist the cap. This guide is that tool.
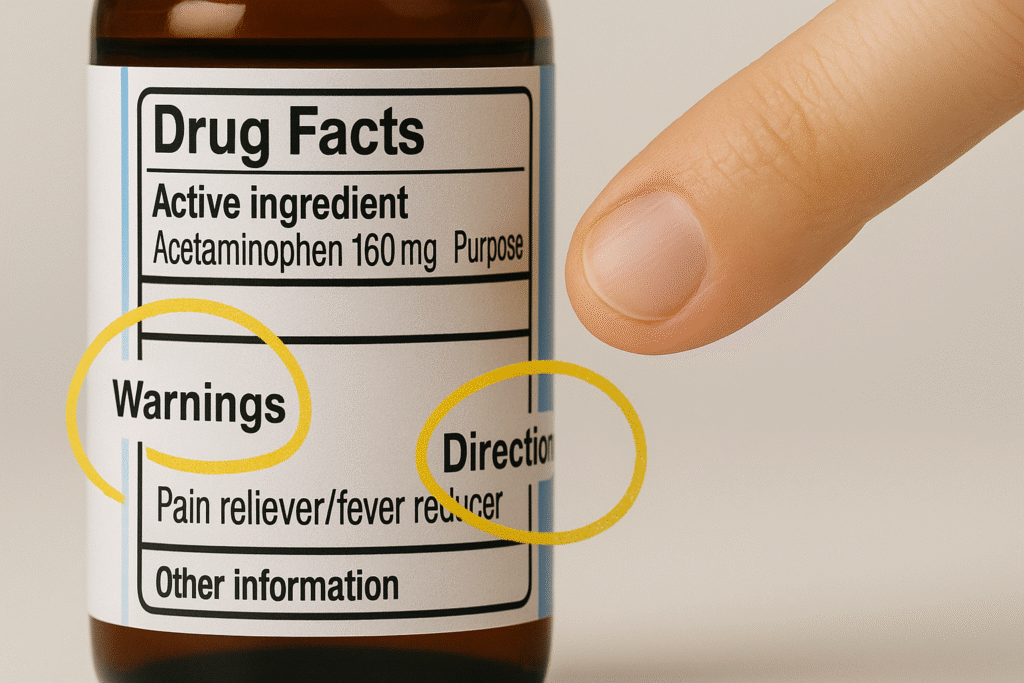
Your First Line of Defense: How to Read a ‘Drug Facts’ Label Like an Expert
The single most important source of safety information for any OTC medicine is printed right on the box: the “Drug Facts” label. The U.S. Food and Drug Administration (FDA) requires this label on all nonprescription medicines, and it’s standardized to have the same format and easy-to-understand language, whether you’re looking at a bottle of cough syrup or a tube of sunscreen.
Think of the ‘Drug Facts’ label as the medicine’s official instruction manual. You wouldn’t try to assemble a new crib without looking at the directions, right? The same principle applies here, but with much higher stakes. You should read this label carefully every single time you give medicine to your child, even if you’ve used the product before, as formulations can change.
Here is a breakdown of what each section means for your child’s safety:
- Active Ingredient(s) & Purpose: This is the “what” and “why” of the medicine. The active ingredient is the component that actually does the work—the part that reduces the fever or quiets the cough. The label will list its name and how much is in each dosage unit (e.g., 160 mg per 5 mL). The purpose tells you what category the drug belongs to, like “Pain reliever” or “Nasal decongestant”. It’s common to see a “brand name” (like Tylenol) and a “generic name” (the active ingredient, like acetaminophen).
- Uses: This section gets more specific, listing the exact symptoms the medicine is designed to treat, such as “temporarily relieves nasal congestion” or “reduces fever”. This helps you match the right product to your child’s specific illness.
- Warnings: This is arguably the most critical section on the label. Read it carefully. It tells you when not to use the product, such as if your child has a specific health condition. It also lists potential side effects, what to avoid while taking the medicine (like other drugs or certain foods), and, most importantly, when you should stop using it and call a doctor.
- Directions: This is the “how-to” guide. It tells you exactly how much medicine to give (the dose), how often to give it, and the maximum amount to give in a 24-hour period. Following these directions precisely is vital to prevent giving too little (which won’t work) or too much (which can be dangerous).
- Other Information: This section provides important details on how to store the medicine properly to keep it safe and effective. Storing it at the wrong temperature, for example, can cause it to break down and lose its potency.
- Inactive Ingredients: These are the other components in the medicine, such as flavorings, dyes, and preservatives, that don’t have a therapeutic effect.6 It is crucial to check this list if your child has any known allergies, as some children may have a reaction to an inactive ingredient like red dye or lactose.
A few practical tips to keep in mind: on smaller bottles, the label may be a peel-back style, so make sure you read all the layers. Always check the expiration date. An expired medicine may not be effective or could even be harmful. If a product has no expiration date, the FDA advises that it should be considered expired three years after it was purchased. Finally, always inspect the packaging for tamper-evident features. If the seal is broken or the package looks damaged, do not use it and return it to the store.
The Active Ingredient as Your North Star
If there is one piece of advice to take away from this entire guide, it is this: focus on the active ingredient, not the brand name. This is the single most important mental shift a parent can make to prevent one of the most common and dangerous medication errors.
Here is how easily a mistake can happen. Imagine your child has a fever. You give them a dose of Children’s Tylenol, which has the active ingredient acetaminophen. A few hours later, their nose is stuffy and they have a cough, so you reach for a multi-symptom cold medicine to help them feel more comfortable before bed. What you may not realize is that many of these combination products, like Dimetapp® Multi-Symptom Cold & Flu,
also contain acetaminophen. Without meaning to, you have just given your child a double dose of the same medication. An overdose of acetaminophen is incredibly dangerous and can cause severe liver damage.
This risk exists because different brands often use the same active ingredients, and a single brand may sell dozens of different products with different combinations of ingredients. The only way to navigate this safely is to make the active ingredient list your North Star. Before giving any medicine, check the active ingredients. If you are giving more than one product, compare their active ingredients to ensure you are not accidentally doubling up. This simple habit is your best defense against accidental overdose.
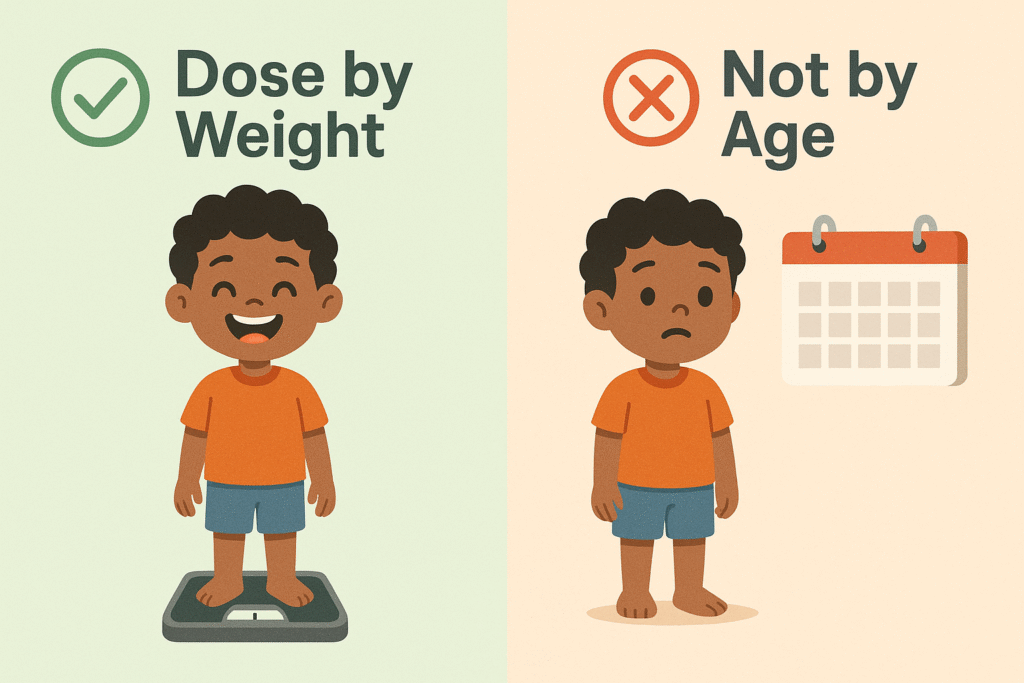
The Dosing Dilemma: Why Your Child’s Weight is the Golden Ticket to Safety
Once you’ve chosen the right medicine, the next critical step is giving the right amount. When you look at the “Directions” on the label, you’ll often see dosing information listed by both age and weight. So, which should you follow? The answer is clear and non-negotiable: always dose based on your child’s current weight.
Dosing by age is like buying a “one-size-fits-all” t-shirt for every 8-year-old in the country. It might fit some kids, but it will be swimming on smaller children and uncomfortably tight on larger ones. Dosing by weight, on the other hand, is like getting that t-shirt perfectly tailored to your child’s exact measurements. It’s the only way to guarantee a safe and effective fit.
This is because a child’s body processes medicine based on its mass, not on how many birthdays they’ve celebrated. Children grow at vastly different rates. A tall, sturdy 4-year-old may weigh significantly more than a petite 4-year-old and may require a different dose to achieve the same therapeutic effect.15 When the label provides a choice, always prioritize the weight-based recommendation. If you don’t know your child’s current weight, get it measured at your pediatrician’s office or use a home scale. Never guess.
It’s also essential to understand the units of measurement. Know the difference between a teaspoon (tsp) and a tablespoon (tbsp), and between milligrams (mg) and milliliters (mL). A tablespoon is three times larger than a teaspoon (1tbsp=15mL; 1tsp=5mL) and confusing the two can easily lead to a dangerous threefold dosing error. And remember, giving more medicine than recommended will not make your child better faster. It only increases the risk of harmful side effects and potential overdose.
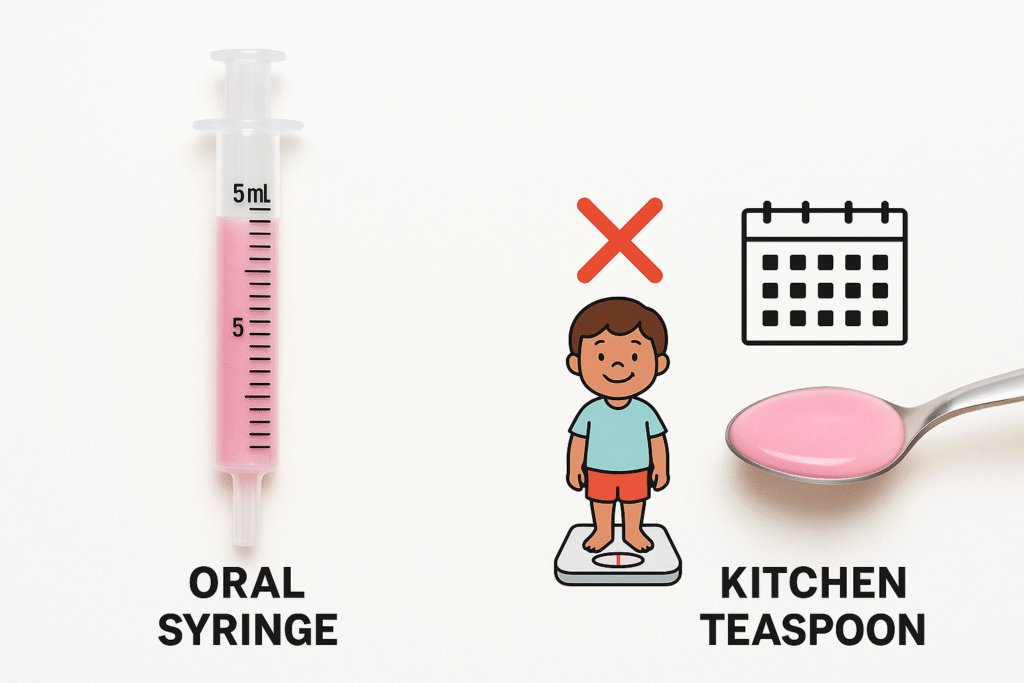
Dosing Accuracy Extends Beyond the Chart to the Tool Itself
The quest for dosing accuracy doesn’t stop once you’ve found the correct amount on the chart. The final, crucial step is using the right tool to measure that dose. Using an improper tool, like a spoon from your kitchen drawer, can completely undermine the precision of weight-based dosing and introduce a significant risk of error.
Here’s why this is so important. Let’s say you’ve carefully checked the label and determined that the correct dose for your child is 5 mL. You might reach for a kitchen teaspoon, assuming it holds exactly 5 mL. The problem is that household spoons are not standardized. Depending on its design, a kitchen “teaspoon” could hold anywhere from 3 mL to 7 mL. This means you could be giving your child up to 40% too little or 40% too much medicine with every single dose.
This seemingly small variation, when repeated every four to six hours, can accumulate. Underdosing can render the medicine ineffective, prolonging your child’s discomfort. Overdosing can increase the risk of side effects and, in some cases, lead to toxicity. Therefore, the principle of accuracy must extend from the chart to the tool. The only way to ensure the precisely calculated dose is delivered is by using the calibrated dosing tool—the syringe, cup, or dropper—that comes with the medicine. This is a non-negotiable step in the chain of medication safety.
Navigating the Pharmacy Aisles: A Deep Dive into Common Children’s Medications
The sheer number of options in the children’s medicine aisle can be dizzying. This section serves as a practical field guide to the most common categories of pediatric OTCs, helping you understand what they do so you can choose the right product for your child’s symptoms.
Taming Fevers and Soothing Pains
For fever and pain, there are two primary, reliable options available over-the-counter. They are the cornerstones of most pediatric medicine cabinets.
- Acetaminophen (Common brand name: Tylenol)
- Ibuprofen (Common brand names: Motrin, Advil)
These medications are both effective pain relievers and fever reducers, but they are different active ingredients that work in different ways. Ibuprofen is part of a class of drugs called nonsteroidal anti-inflammatory drugs (NSAIDs), which means it can also help reduce inflammation associated with things like sprains or ear infections. Acetaminophen does not have a significant anti-inflammatory effect.
There are a few key differences to be aware of. Ibuprofen is generally not recommended for infants under 6 months of age. Both are safe when used as directed, but overdosing can be dangerous in different ways: taking too much acetaminophen can cause serious liver damage, while taking too much ibuprofen can harm the stomach and kidneys.
Some parents and pediatricians use a strategy of alternating between acetaminophen and ibuprofen to manage a stubborn fever. For example, you might give a dose of ibuprofen, and then three hours later, if the fever is still high, give a dose of acetaminophen. This should only be done after consulting with your child’s healthcare provider.
To ensure you are giving the correct dose, please refer to the following weight-based chart.
Table 1: Pediatric Dosing Chart for Acetaminophen & Ibuprofen
| Child’s Weight | Acetaminophen (160 mg/5 mL) | Ibuprofen (100 mg/5 mL) |
| 6-11 lbs | 1.25 mL | DO NOT USE under 6 months |
| 12-17 lbs | 2.5 mL | 2.5 mL |
| 18-23 lbs | 3.75 mL | 3.75 mL |
| 24-35 lbs | 5 mL | 5 mL |
| 36-47 lbs | 7.5 mL | 7.5 mL |
| 48-59 lbs | 10 mL | 10 mL |
| 60-71 lbs | 12.5 mL | 12.5 mL |
| 72-95 lbs | 15 mL | 15 mL |
| 96+ lbs | 20 mL | 20 mL |
Note: This chart is for informational purposes. Always follow the directions on the product label or from your pediatrician. Do not give ibuprofen to children under 6 months old. Do not give acetaminophen to children under 12 weeks old without consulting a doctor.
Decoding Coughs and Colds
The aisle for children’s cough and cold medicine is perhaps the most confusing of all. Before you even consider buying one of these products, you must be aware of this critical warning from the FDA and the American Academy of Pediatrics: Do NOT give OTC cough and cold medicines to children under the age of 4. For children aged 4 to 6, these products should only be used if specifically recommended by your doctor.
Why such a strong warning? Research has shown that these medications are often ineffective in young children and, more importantly, they carry the risk of serious side effects, including rapid heart rate, convulsions, and in rare cases, can be fatal.
The names on the boxes—”Multi-Symptom,” “Daytime,” “Nighttime”—are marketing terms. To make a safe choice for an older child, you must understand the active ingredients inside.
Table 2: Common Cough & Cold Ingredients
| Ingredient Class | What It Does | Common Active Ingredients | Found In Brands Like |
| Cough Suppressant | Reduces the cough reflex. Best for dry, hacking coughs. | Dextromethorphan | Robitussin® DM, Delsym®, Children’s SUDAFED PE® Cold + Cough |
| Expectorant | Thins and loosens mucus, making coughs more productive. | Guaifenesin | Mucinex®, Robitussin® |
| Decongestant | Shrinks swollen nasal passages to relieve stuffiness. | Phenylephrine, Pseudoephedrine | Sudafed®, Sudafed PE® |
| Antihistamine | Dries up a runny nose and can cause drowsiness. | Diphenhydramine, Chlorpheniramine, Brompheniramine | Benadryl®, Dimetapp®, Triaminic® |
Given the risks and limited benefits, it’s often safer and more effective to rely on non-medicinal remedies, especially for young children. These include:
- Hydration: Offer plenty of fluids like water and warm broth to keep them hydrated and thin mucus.
- Honey: For children over 1 year old, a teaspoon of honey can soothe a cough. NEVER give honey to an infant under 1 year old due to the risk of infant botulism.
- Saline and Suction: Use saline nasal spray or drops to loosen mucus, then a bulb syringe or nasal aspirator to clear your child’s nose, especially before feeding and sleeping.
- Humidifier: A cool-mist humidifier in your child’s room can add moisture to the air and ease congestion. Avoid warm-mist humidifiers, which pose a burn risk.
Managing Allergies: From Sneezes to Sprays
For children suffering from seasonal or environmental allergies, OTC medications can provide significant relief. The options generally fall into three categories.
- Nondrowsy/Less-Drowsy Antihistamines: These are the recommended first-choice for treating allergy symptoms like sneezing, itchy eyes, and runny nose. They are effective and generally well-tolerated. Common options include cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra).
- Older, Drowsy Antihistamines: The most common of these is diphenhydramine (Benadryl). While it is a very effective and fast-acting antihistamine, it causes significant drowsiness. For this reason, it’s often found in “nighttime” cold and allergy formulas and is typically used for more acute reactions like hives rather than daily allergy management.
- Steroid Nasal Sprays: For children with persistent allergy symptoms, especially nasal congestion, steroid nasal sprays can be highly effective. These work by reducing inflammation in the nasal passages. They may take a few days to reach their full effect. Common options include fluticasone (Flonase) and triamcinolone (Nasacort).
Table 3: A Guide to Pediatric Allergy Medications
| Active Ingredient | Common Brand Name | Type | Typical Age Recommendation |
| Cetirizine | Zyrtec® | Oral Antihistamine | 2 years and older |
| Loratadine | Claritin® | Oral Antihistamine | 2 years and older |
| Fexofenadine | Allegra® | Oral Antihistamine | 2 years and older |
| Diphenhydramine | Benadryl® | Oral Antihistamine (Drowsy) | Check label; often 6+ years |
| Fluticasone | Flonase® | Steroid Nasal Spray | 2-4 years and older (depending on product) |
| Triamcinolone | Nasacort® | Steroid Nasal Spray | 2 years and older |
Note: Always check the product label for specific age and dosing instructions. For children under 2, consult a doctor before giving any allergy medication.
The “Never-Ever” List: Critical Warnings Every Parent Must Know
Some medication risks are so significant that they deserve their own section. These are the absolute “never-ever” rules of pediatric OTC safety.

The Aspirin Alert: Understanding Reye’s Syndrome
This is the most important warning in pediatric medicine. NEVER, ever give aspirin to a child or teenager who is recovering from a viral illness like the flu or chickenpox.
This is because of the link to Reye’s syndrome, a rare but devastating and potentially fatal illness that causes sudden swelling in the liver and brain. The symptoms can appear suddenly and progress rapidly, including persistent vomiting, lethargy, confusion, and seizures.
To keep your child safe, avoid aspirin entirely for fever and pain. Stick to acetaminophen or ibuprofen. Be a label detective: aspirin can also be listed as “acetylsalicylic acid” or “salicylate,” and it can be a hidden ingredient in some products, like certain upset stomach remedies. The only exception to this rule is if a doctor has prescribed aspirin for a specific chronic condition, such as Kawasaki disease.
The Hidden Danger of “All-in-One” Medicines
Multi-symptom or “all-in-one” cough and cold medicines may seem like a convenient solution, but they often pose more risks than benefits, especially for children.
Think of it this way: using a multi-symptom medicine when your child only has a stuffy nose is like using a Swiss Army Knife with every single tool opened just to tighten one screw. You’re far more likely to cause unnecessary problems (like side effects from ingredients they don’t need) than to solve the one specific issue you’re facing. It is always safer and more effective to use a simple screwdriver—a single-ingredient medicine that targets only the symptom your child actually has.
The biggest risk, as mentioned before, is accidental overdose. These products often contain a pain reliever/fever reducer like acetaminophen or ibuprofen. If you give one of these products and then also give a separate dose of Tylenol or Motrin, you are dangerously doubling up on that active ingredient. The safest approach is to identify your child’s primary symptom—a cough, a stuffy nose, or a fever—and choose a medicine that treats only that.
The Practical Side of Safety: Tools, Storage, and Disposal
Medication safety goes beyond choosing the right product and dose. It extends to the practical, everyday habits of how you measure, store, and dispose of medicines.
Beyond the Kitchen Spoon: Using the Right Dosing Tools
We’ve touched on this, but it bears repeating: never use a kitchen spoon to measure medicine.
They are not accurate and can lead to significant dosing errors.
Always use the calibrated dosing tool that is packaged with the medicine. This could be:
- An oral syringe, which is the most accurate tool, especially for small doses under 5 mL.
- A dosing spoon with clear mL markings.
- A dosing cup with printed measurement lines.
When using these tools, be meticulous. Place a dosing cup on a flat surface to read it at eye level. With a syringe, carefully draw the liquid to the correct mL line. Pay close attention to decimal points—a dose of “0.5 mL” is ten times smaller than “5 mL,” and a mix-up can be dangerous.
Fort Knox for Your Medicine Cabinet: Safe Storage Strategies
Children are naturally curious explorers. To them, a small, colorful pill can look just like candy. That’s why safe storage is a critical, non-negotiable part of protecting them.
Think of your medicine storage like a fire extinguisher: it needs to be in a specific, known place that adults can easily access but is completely off-limits to children. A high, locked cabinet is the gold standard for safety.
Here are the key rules for safe storage:
- Up, Away, and Out of Sight: Store all medicines—prescription, OTC, vitamins, and even things like medicated creams and mouthwash—in a high location that a child cannot see or reach.
- Use Original Containers: Keep medicines in their original bottles with the safety caps tightly secured. But remember, “child-resistant” does not mean “child-proof.” A determined toddler can often figure out how to open them, which is why out-of-reach storage is so vital.
- Put It Away Immediately: After every single use, put the medicine back in its safe storage spot. Never leave it on a kitchen counter, a nightstand, or in a diaper bag where a child could find it.1
- Mind the Visitors: Be mindful of medications in the purses or bags of visitors, like grandparents or babysitters. Kindly ask them to keep their bags out of your child’s reach.
- Never Call It “Candy”: To entice a reluctant child, you might be tempted to call medicine “candy.” Never do this. It sends a confusing and dangerous message that could lead them to seek out and ingest medicine on their own.
Responsible Disposal
When a medicine is expired or no longer needed, it’s important to dispose of it properly. Check to see if your community has a “drug take-back” program, often located at pharmacies or police stations. If not, the safest way to dispose of most medicines is to mix them (do not crush tablets) with an unappealing substance like used coffee grounds or cat litter, place the mixture in a sealed plastic bag, and throw it in your household trash.
When to Worry: Your Emergency Action Plan
Even with the best precautions, accidents can happen. And sometimes, an illness is more serious than an OTC medicine can handle. It is crucial to know what to do in an emergency and to recognize the “red flag” symptoms that mean you should bypass the medicine cabinet and call a professional immediately.
What to Do in Case of an Accidental Overdose
If you suspect your child has taken the wrong medicine or too much of a medicine, the first step is to stay calm but act quickly.
- Do not try to make your child vomit.
- Immediately call the Poison Control Hotline at 1-800-222-1222. This national hotline is free, confidential, and staffed 24/7 by poisoning experts. Save this number in your phone right now.3
- Have this information ready: When you call, be prepared to provide the child’s age and weight, the name of the medicine (have the bottle in your hand), the amount you think was taken, and the time it was taken.
- Call 911 instead if your child is unconscious, having a seizure, having severe trouble breathing, or is unresponsive. These are signs of a medical emergency that requires immediate help.
Red Flags: When to Call the Doctor Immediately
One of the hardest parts of being a parent is knowing when to worry. You’re often told to “trust your instincts,” but in a moment of stress, that can be difficult. This section is designed to give you concrete, objective data to back up your instincts. It provides a clear checklist of “red flag” symptoms that should prompt you to call your doctor or seek emergency care. Seeing one of these symptoms transforms a subjective worry (“my child just seems really sick”) into an objective reason to act (“my child has a fever and a stiff neck, which requires an immediate call”). This empowers you to make confident decisions and ensures your child gets the care they need, when they need it.
From Worried to Well-Prepared
Navigating the world of children’s health can feel like a monumental responsibility, but you are more than capable of handling it. The golden rules of OTC medication safety are simple but powerful: read the label every time, focus on the active ingredient, dose by your child’s weight, use the right measuring tool, store all medicines safely, and know the red flags that signal it’s time to call for help.
By taking the time to read this guide, you have already taken the single most important step in protecting your child. You have armed yourself with knowledge, which is the best medicine of all. You are no longer just a worried parent in a pharmacy aisle; you are a well-prepared caregiver, ready to manage your child’s common illnesses with safety, skill, and confidence.
Now, take these final two steps to complete your safety toolkit:
- Save the Poison Control number (1-800-222-1222) in your phone right now. You hope you’ll never need it, but if you do, you’ll be glad it’s there.
- Share this guide. Send it to anyone who cares for your child—grandparents, babysitters, family, and friends. Creating a consistent circle of safety around your child is the ultimate act of love and protection.



